LMB-CO63
Stride4®
The Stride4® is a mechanical stance control orthotic knee joint that utilizes a low-profile cabling system to automatically unlock at the end of stance phase. At the end of swing phase, when the orthotic knee joint reaches full extension, the locking mechanism reengages to provide knee stability for stance phase. Cable adjustment clevises allow the practitioner to easily adjust the cable length to match the patient's stride length. The joint body of the Stride4® is comprised of a four bar linkage mechanism; the upper and lower aspects of the joint do not purely rotate about one fixed center of rotation. Instead, the joint motion involves some translation, in addition to rotation, to more closely mimic anatomical knee motion. In the stance control mode of operation, the four bar linkage mechanism provides stability when the orthotic knee joint is fully extended. An integral extension assist spring housed within the midsection assists with knee extension, while an adjustable extension stop allows the practitioner to adjust and fine tune the point at which the joint enters into its stable/locked state. If desired, the extension stop can be fully adjusted to eliminate the stability feature to facilitate free motion. A button on the Stride4® allows the patient to switch between locked and stance control modes of operation. This feature provides the patient with the option of locking the joint should they desire. When the lock option is selected and engaged by the patient, the joint will allow approximately 3° of flexion to provide some shock absorption to the user.
For more and information please visit our product spotlight page.
Knee Joint Selection Guide
Discretion in choosing a joint size and designing an appropriate orthosis should be used by the orthotist in all cases. We would reference and support the approach described by Lunsford and agree that successful orthotic management requires a clear understanding of the condition being treated and a realistic plan to address the biomechanical deficits presented.
For optimal orthotic management, the mechicanical demands to be placed upon the orthosis for any given treatment must be understood prior to material selection.
The selection of the correct materials is often the difference between success and failure and we believe that the orthotist is trained and the best qualified to match the characteristics of the material to the biomechanical and functional needs of the patient.
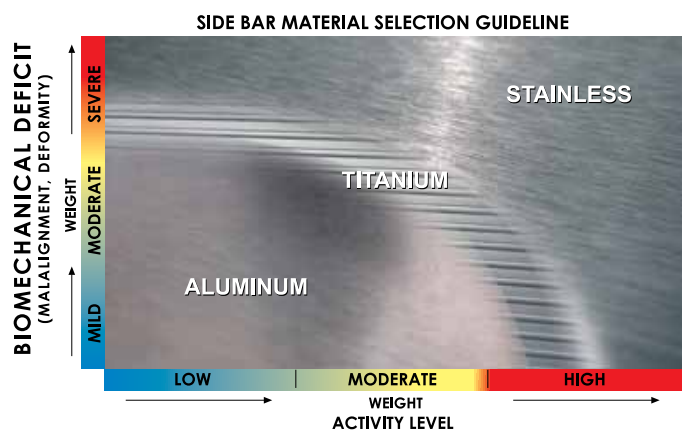
Discretion in choosing a joint size, selecting the Side Bar Material, and designing an appropriate orthosis should be used by the orthotist in all cases. The following factors are commonly used by orthotists to help determine the level of Biomechanical Deficit. Practical issues including compliance, occupation, environment and social factors should also be taken into consideration.
Biomechanical Deficit Factors
- Single or multiple plane involvement
- Single or multiple segment involvement
- Muscle strength/weakness
- Range-of-motion
- Skeletal and/or joint alignment — malalignment
- Mobile or fixed deformity
- Presence and magnitude of joint contracture
- Presence/extent of spasticity
- Proprioceptive and cognitive skills
- Progressive or non progressive condition
Steel and Aluminum Alloys
Steel is stronger and stiffer than aluminum allow; aluminum allow has a lower density making it lighter. Steel is fatigure resistant and combines high rigidity, or ductility depending on the alloy. The main disadvantage of steel is its weight. The major benefit of aluminum in orthotics is its high strength to weight ratio. Aluminum does however have a lower endurance limit under repreated dynamic loading conditions than does steel. A common clinical question relates to the upright of a lower extremity orthosis in which deformation under bending stresses is very important. In general terms, if loading conditions are known to be great or highly repetitive, steel is superior to aluminum.
Considerations for preventing failure:
- Fatigue
- Stress Concentration
- Finishing
- Bend Radii
- Design


 Downloadable Version
Downloadable Version